Course Material – Engage Patients in Your Antibiotic Stewardship Program
Clinical Focus
- Discovery of antibiotics over the past century has changed the field of medicine beyond any other discovery to date
- Antibiotics are powerful drugs that have transformed health care around the world – making once deadly diseases treatable and saving millions of lives
- Antibiotics are the foundation of modern medicine
- Antibiotics are relied upon to treat people with the most serious infections, such as pneumonia or sepsis, and those at high risk for developing infections
- Unfortunately, overuse and misuse of antibiotics have resulted in increasing resistance, creating the real and growing threat of new “super-bugs” that are increasingly difficult to treat
- Studies indicate that 30-50% of antibiotics prescribed in hospitals are unnecessary or inappropriate
Patients Most at Risk for Severe Infections
- Surgery – patients undergoing any type of surgery, including cardiac bypass and joint replacement, are at risk of surgical site infections
- Dialysis for end-stage renal disease – infection risk is high in patients with ESRD (a condition in which kidneys are no longer working) because the patients have weakened immune systems and dialysis requires access to their bloodstream
- Cancer chemotherapy – patients are often at risk for developing serious infections because the treatment weakens their immune systems
- Inflammatory conditions – patients with inflammatory conditions, such as rheumatoid arthritis and inflammatory bowel disease are treated with medicines that can be associated with increased risk of infection
- Organ transplants – patients receiving organ transplants are at high risk for infections because they may undergo complex surgery and most receive medicines that weaken their immune system as part of their treatment

Established Risk of Antibiotic Use
- Increased infection risk – Though used to treat infections, they can also increase the risk of some types of infection such as C. difficile and Candida
- Allergic reactions – Can range from mild rashes and itching to life threatening swelling of the face and throat and anaphylaxis
- Drug interactions – Can interact with other drugs patients take making antibiotics less effective or giving the patient worse side effects
- Antibiotic resistance – The bacteria might adapt to develop new resistance against the drug and cause resistant infections in that patient and/or spread to other people
Improving Antibiotic Use to Combat Resistance

- It is a national priority to improve the use of antibiotics in healthcare to protect patients and reduce the threat of antibiotic resistance
- Improving the way healthcare professionals prescribe antibiotics, track antibiotics, and the way we take antibiotics, helps keep us healthy now, helps fight antibiotic resistance, and ensures that these life-saving drugs will be available for future generations
- www.cdc.gov/antibiotic-use
Antibiotic Resistance
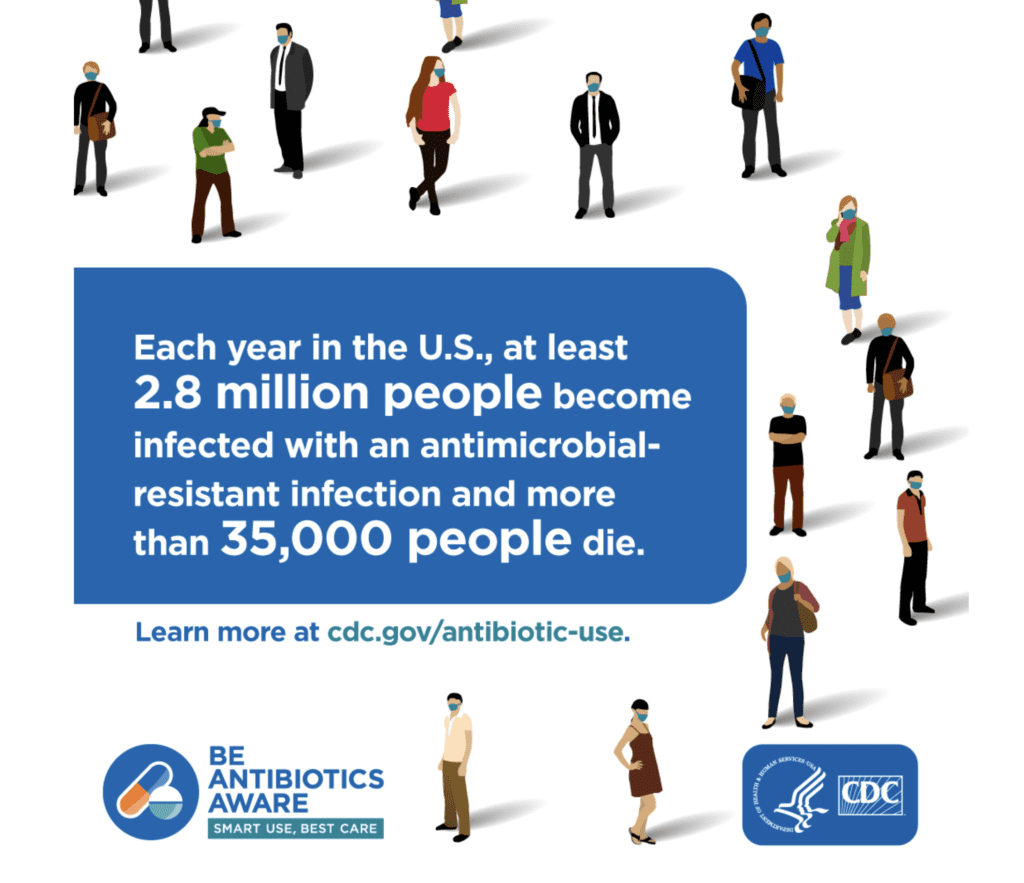
- Antibiotic resistance is one of the most urgent threats to the public health
- Each year in the U.S., at least 2 million people get infected with antibiotic-resistant bacteria. At least 23,000 people die as a result
- Antibiotic resistance does not mean the body is becoming resistant to antibiotics; it is that bacteria develop the ability to defeat the antibiotics designed to kill them
- When bacteria become resistant, antibiotics cannot fight them, and the bacteria multiply
- Some resistant bacteria can be harder to treat and can spread to other people
Antibiotic Stewardship

- Antibiotic Stewardship is the effort
- To measure antibiotic prescribing
- To improve antibiotic prescribing by clinicians and use by patients so that antibiotics are only prescribed and used when needed
- To minimize misdiagnoses or delayed diagnoses leading to underuse of antibiotics
- To ensure that the right drug, dose and duration are selected when an antibiotic is needed
- Goal of antibiotic stewardship is to maximize the benefit of antibiotic treatment while minimizing the harm both to individual persons and to communities
Antibiotics Aren’t Always the Answer
Everyone has a Role in Improving Antibiotic Use
- Healthcare Providers
- Patients and Families
- Health Systems (hospitals, clinics, nursing homes)
- Healthcare Quality Organizations
- Health Insurance Companies
- Healthcare Provider Professional Organizations
- Federal, State, and Local Health Agencies
Healthcare Providers
- Follow clinical guidelines when prescribing antibiotics – Remember to prescribe the right antibiotic, at the right dose, for the right duration, and at the right time
- Protect your patients, only prescribe antibiotics when needed; You can do harm by prescribing antibiotics that aren’t needed
- Place written commitments supporting antibiotic use in exam rooms to help facilitate patient communication
- Tell your patients why they don’t need antibiotics for viral infection, what to do to feel better, and when to seek help if they don’t feel better
- Talk to your patient and families about the possible harms from antibiotics, such as allergic reactions, C. difficile, and antibiotic-resistant infections
- Review antibiotic therapy 48-72 hours after started and change orders as needed – a critical step in care
- Watch for sign of sepsis (confusion, shortness of breath, high heart rate, fever or shivering, extreme pain, clammy or sweaty skin) and start antibiotics immediately
- Be aware of antibiotic resistance pattern in your facility and community; use data for prescribing
- Follow hand hygiene and other infection prevention measures on every patient
Patients and Families
- Talk to healthcare provider about when antibiotics will and won’t help, ask about antibiotic resistance
- Talk to healthcare provider about how to relieve symptoms
- Ask what infection an antibiotic is treating, how long antibiotics are needed, and what side effects might happen
- Take antibiotics only when prescribed and exactly as prescribed
- Don’t save an antibiotic for later or share the drugs with someone else
- Insist that everyone cleans their hands before touching you
- Stay healthy and keeps others healthy be cleaning hands, covering coughs, staying home when sick, and getting recommended vaccines
- Get vaccinated for flu and pneumonia
Symptom Relief Suggestions

- Pain relievers
- Fever reducers
- Saline nasal spray or drops
- Warm compresses
- Liquids
- Rest
Health Systems, Hospitals, Clinics, and Nursing Homes
- Adopt and implement antibiotic stewardship policies and strategies, including CDC’s Core Elements of Antibiotic Stewardship
- Designate staff members to coordinate antibiotic stewardship activities
- Monitor antibiotic prescribing data to identify areas for improvement, and assess the impact of antibiotic stewardship areas
- Educate staff about antibiotic resistance and strategies to optimize antibiotic prescribing
Healthcare Quality Organizations
- Develop and implement standards requiring antibiotic stewardship programs and practices
- Develop and adopt standards measuring the success of antibiotic stewardship programs and practices
Health Insurance Companies
- Incentivize implementation of antibiotic stewardship programs and practices
- Use clinical performance data on quality measures for appropriate prescribing, such as the Healthcare Effectiveness Data and Information Set (HEDIS)measures
Healthcare Provider Professional Organizations
- Create and share clinical practice guidelines for the diagnosis and management of common conditions
- Incorporate antibiotic stewardship principles into antibiotic use guidelines
- Provide continuing medical education opportunities about antibiotic stewardship for members
- Bolster nation, local, and regional initiatives promoting appropriate antibiotic prescribing and use
- Highlight new research and technologies to support antibiotic stewardship
Federal, State, and Local Health Agencies
- Set expectations for the implementation of antibiotic stewardship activities across the spectrum of health care
- Provide data and tools to help guide stewardship activities
- Connect local stakeholders and coalitions
- Support partners, healthcare providers, and patients through development and dissemination of educational resources
- Support innovations and research, such as diagnostic test development, that facilitate optimal antibiotic use
What Do We Know About Antibiotic Use In Outpatient Settings?
- In 2015 alone, approximately 269 million antibiotic prescriptions were dispensed from outpatient pharmacies in the U.S.
- Enough for five out of six people to receive one antibiotic prescription each year
- At least 30% were unnecessary
- Most unnecessary prescriptions are for respiratory conditions most commonly caused by viruses that do not respond to antibiotics
- Data show that antibiotics are prescribed more frequently in states in the Southern and Appalachian regions
- Prescribing the correct antibiotic is another area that needs attention – patients often prescribed antibiotic not recommended by current clinical guidelines
- Family practice physicians prescribe the most antibiotics
Core Elements of Outpatient Antibiotic Stewardship
- Commitment – Demonstrate dedication to and accountability for optimizing antibiotic prescribing and patient safety
- Action for policy and practice – Implement at least one policy or practice to improve antibiotic prescribing, assess whether it is working, and modify as needed
- Tracking and reporting – Monitor antibiotic prescribing practices and offer regular feedback to providers, or have providers assess their own antibiotic prescribing practices
- Education and expertise – Provide educational resources to providers and patients on antibiotic prescribing, and ensure access to needed expertise on optimizing antibiotic prescribing
Audience for Outpatient Antibiotic Stewardship

- Primary care clinics and providers
- Outpatient specialty and subspecialty clinics and providers
- Emergency departments and emergency medicine providers
- Retail health clinics and providers
- Urgent care clinics and providers
- Dental clinics and dentists
- Nurse practitioners and physician assistants
- Healthcare systems
- Patients and their families
Antibiotic Stewardship Programs and Activities Can:
- Improve patient outcomes – By reducing unnecessary antibiotic prescribing, antibiotic stewardship programs and activities can improve the treatment of infections and prevent avoidable side effects, reactions, and other problems for patients
- Decrease C. Difficile infections – By reducing the use of high-risk antibiotics
- Decrease antibiotic resistance – Preventing infections and improving antibiotic prescribing could save 37,000 lives from antibiotic resistant infections over 5 years
- Decrease Costs – They have consistently demonstrated annual savings of $200,000 to $400,00 in hospitals and other healthcare facilities
Patient Engagement
To learn more about antibiotic prescribing and use, visit: www.cdc.gov/antibiotic-us
- Engaging patients is critical to the effort to improve antibiotic use
- Helping patients know what they can do to keep themselves and their loved ones safe is part of the discussion of improving antibiotic use
- This means raising awareness about the side effects of antibiotics, as well as the unintended consequences of antibiotic use
- CDC’s new and existing education efforts will work to ensure that antibiotics are used properly and that patients that might have sepsis are recognized and started on antibiotic quickly, and reassessed within 48 hours when the patient’s culture results are back
Patient Involvement and Empowerment

- Get the facts about antibiotics. Antibiotics do not work on viruses, such as colds and flu, or runny noses, even if the mucus is thick, yellow or green. When antibiotics aren’t needed, they won’t help you, and the side effects could still hurt you
- Ask doctor or nurse about the best way to feel better while your body fights off a virus (pain relievers, fever reducers, saline nasal spray or drops, warm compresses, liquids and rest may help)
- If you need antibiotics, take them exactly as prescribed. Talk with your doctor if you have questions about your antibiotics, or if you develop any side effects
- Stay healthy and keep others healthy by cleaning hands, covering coughs, staying home when sick, and getting the recommended vaccines, (e.g. for flu)
- Patient and families are encouraged to use the education materials and learn more about antibiotics – www.cdc.gov/antibiotic-use
Patient and Family Education
Communicate strategies to educate patients about when antibiotics are and are not needed
- Inform that antibiotic treatment for viral infections provides no benefit
- Inform that certain bacterial infections (mild ear, sinus) might improve without antibiotics
- Provide recommendations for when to seek medical care if symptoms worsen or do not improve
Educate patients about the potential harms of antibiotic treatment
- Common and serious side effects
- Evidence suggests that use in infancy and childhood is linked with allergic, infectious, and autoimmune diseases
Provide patient education materials
- Information on appropriate antibiotic use, adverse drug events, and resources regarding symptomatic relief for common infections
- CDC http://www.cdc.gov/getsmart
Leadership Commitment
- Dedicating necessary human, financial and information technology resources
- Write statements in support of improving antibiotic use to be shared with staff and families
- Include stewardship-related duties in position job descriptions
- Communicate with nursing staff and prescribing clinicians the facilities’ expectations about use, monitoring, and enforcement of stewardship policies
- Create a culture through messaging, education and celebrating improvement, which promotes stewardship
In Summary
- Efforts to improve antibiotic use will succeed only if everyone plays a role
- Antibiotics save lives. – When a patient needs antibiotics, the benefits outweigh the risks of side effects and antibiotic resistance.
- Improving the way we take antibiotics helps keep us healthy now, helps fight antibiotic resistance, and ensures that life-saving antibiotics will be available for future generations
Citations
- CDC. Antibiotic Use in the United States, 2017: progress and Opportunities. Atlanta, GA: US Department of Health and Human Services, CDC; 2017.
- Sanchez, G.V., Fleming-Dutra, K.E., Roberts, R.M., Hicks, L.A. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm Rep 2016;65(No. RR-6):1-12
- CDC. The Core Elements of Antibiotic Stewardship for Nursing Homes. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. Available at: http://cdc.gov/longtermcare/index.html
- CDC. Core Elements of Hospital Antibiotic Stewardship Programs. Atlanta, GA: US Department of Health and Human Services, CDC: 2014. Available at: http://www.cdc.gov/getsmart/healthcare/implementation/core-elements.html
- National Quality Forum: Antibiotic Stewardship in Acute Care
- www.qualityforum.org
- www.cdc.gov/antibiotic-use
